![]()
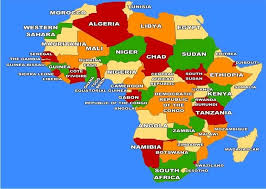
Across Africa, we have an uncomfortable habit: we treat mental health medication like a “nice-to-have” instead of what it often is: the difference between stability and crisis. Many patients start treatment, feel better, then stop. Others ration tablets to make them last, skip doses when money is tight, or abandon treatment when relatives insist the illness is spiritual. Some stop because side effects are real and frightening. The result is predictable: relapse, disrupted schooling and work, family breakdown, avoidable hospital admissions, and even harm. Medication adherence is not about blind obedience to doctors. It is about respecting how these conditions behave. Disorders like schizophrenia, bipolar disorder, and severe depression are frequently chronic or recurrent. When medication is prescribed, it is usually because your clinician believes the benefits outweigh the risks for your specific situation. The World Health Organization’s mhGAP guidance in 2016 repeatedly emphasizes monitoring adherence and ensuring continuity of care because ongoing treatment is central to long-term outcomes, especially for psychosis and bipolar disorder.
Let’s be direct: stopping psychiatric medication abruptly is one of the fastest routes back to symptoms. That is not “weak faith” or “lack of discipline.” It is biology, relapse risk, and illness course. Research consistently links non-adherence to symptom relapse, re-hospitalization, and poorer functioning. A study by Addisu et al in 2025 on antipsychotic non-adherence summarizes these consequences bluntly: relapse and readmission are common downstream effects when people don’t take antipsychotic medication as prescribed. And Africa-specific evidence in 2017 shows the problem is not rare; studies among Nigerians living with schizophrenia, for example, have documented substantial non-adherence and its association with worse outcomes and quality of life.
So why do people stop? Because we don’t make adherence easy or realistic. The first reason is side effects. Sedation, weight gain, sexual dysfunction, tremor, restlessness: these are not “small issues.” They can wreck confidence and relationships. But the self-sabotage is suffering silently and quitting without telling your clinician. The practical move is to report side effects early and specifically. Many can be managed by dose adjustment, switching medicines, changing timing (night vs morning), adding a side-effect remedy, or choosing a different formulation. Quitting in secret protects nobody. The second is cost and supply. Missed doses are often structural, not personal. If a clinic frequently runs out of medicines, if transport costs are crushing, or if a patient must choose between food and tablets, “just comply” is an empty slogan. Health systems must do better. But patients can still reduce risk: plan refills before you run out, ask the clinic what alternatives exist when a brand is unavailable, and discuss longer-duration options where appropriate (including long-acting injectable antipsychotics for some patients). The next one is stigma and misinformation. In many communities, the most dangerous sentence is: “You look fine now, stop the drugs.” Looking fine is often the result of treatment. The same stigma that makes people hide their diagnosis also makes them skip doses to avoid being “seen” taking medication. If you have a trusted family member, spouse, or friend, recruit them as an adherence ally, not as a policeman, but as support for reminders, appointments, and early warning signs. Lastly, there are spiritual and traditional interpretations. You can hold spiritual beliefs and still take medication. The real question is whether your belief system helps you stay stable or pushes you into cycles of relapse. A hard truth: any advisor (religious or traditional) who tells you to stop prescribed medication without coordinating with your clinician is gambling with your brain, your safety, and your future. If you want prayer, deliverance, or traditional support, fine. Combine it with medical care, don’t replace it.
Here are practical habits that actually work:
1. Tie medication to a daily anchor: after brushing, with breakfast, after evening prayers, same cue every day.
2. Use a pillbox and alarms. Not because you’re careless, but because memory and routine break under stress.
3. Track your “relapse signature”: sleep changes, irritability, suspiciousness, racing thoughts, withdrawal. Share it with someone close.
4. Never stop suddenly. If you want to stop or change, take that desire to your clinician and do it safely.
5. Make appointments non-negotiable. Medication without follow-up is guesswork; follow-up is where doses are refined and side effects are handled.
This is the editorial point Africa and Nigerians needs to hear: adherence is not a moral issue. It is a strategy. Taking medication as prescribed is often the most practical form of self-respect a mental health patient can practice since stability is the platform on which everything else stands. If we want fewer people chained to recurrent crises, we must stop romanticizing “stopping drugs” as bravery. In mental health, consistency is bravery.